Knee Arthritis
Arthritis
- Arthritis is wear and tear of the cartilage of a joint:
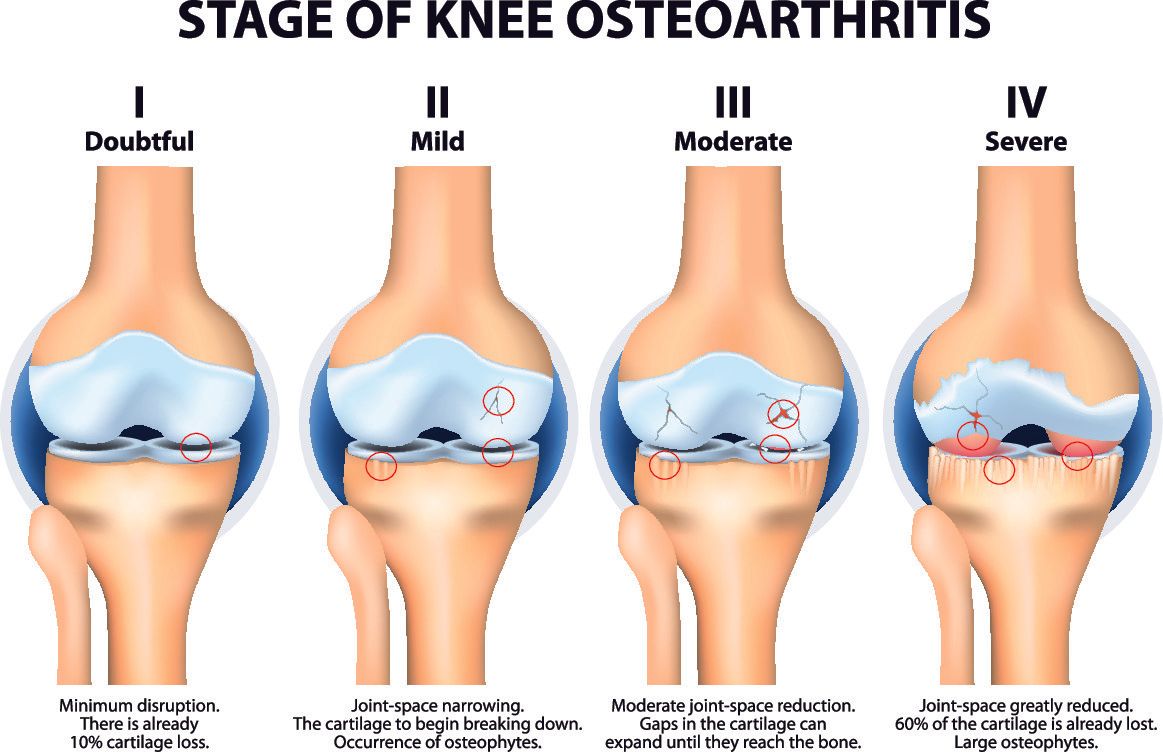
- The normal smooth surface of articular cartilage become rough, losing its cushioning properties and when advanced then the underlying bone is exposed
- There are two main types of arthritis:
- Osteoarthritis (most common)
- Inflammatory arthritis (the most common type being rheumatoid arthritis)
- Osteoarthritis can be of two types:
- Primary:
- The most common variety
- Not triggered or caused by anything specifically
- Due to wear and tear as get older
- Occasionally can be found in multiple family members suggesting genetic cause
- Tends to present after 55 years of age
- If live long enough everybody would be affected by it
- Secondary:
- Less common
- Triggered by a specific cause such as obesity, trauma, sports related, heavy manual labour, abnormal leg alignment, joint inflammation, knee instability, sedentary lifestyle
- Osteoarthritis can affect other joints such as hands, feet, spine and hips
- Osteoarthritis is the single most common cause of disability in older population
- 10-15% of all adults over 60 have a degree of osteoarthritis
- More common in women than men
Symptoms
- Pain:
- Often described as a dull achy pain made worse during or after walking/exercise
- When arthritis is more advanced patients often wake up from sleep due to the pain
- Stiffness:
- the knee joint starts to lose its full range of motion
- Due to pain, patients tend to avoid moving the knee and so the surrounding soft tissues (capsule, muscles, tendons, ligaments) contract and tighten up making movement more painful
- Creaking and grinding:
- Felt when moving the knee due to the rough surfaces rubbing against each other
- Swelling:
- As the overlying cartilage wears away and the underlying bone is exposed, excess synovial fluid is produced (called an effusion) so as to help reduce the friction caused by the rough surface of the exposed bone
- Mechanical symptoms:
- Patients have a sensation of catching, locking, or giving way due to a degenerate meniscal tear or loose cartilage bodies
- Difficulties with activities of daily living:
- Walking, going up and down stairs, bending and kneeling down
Investigations
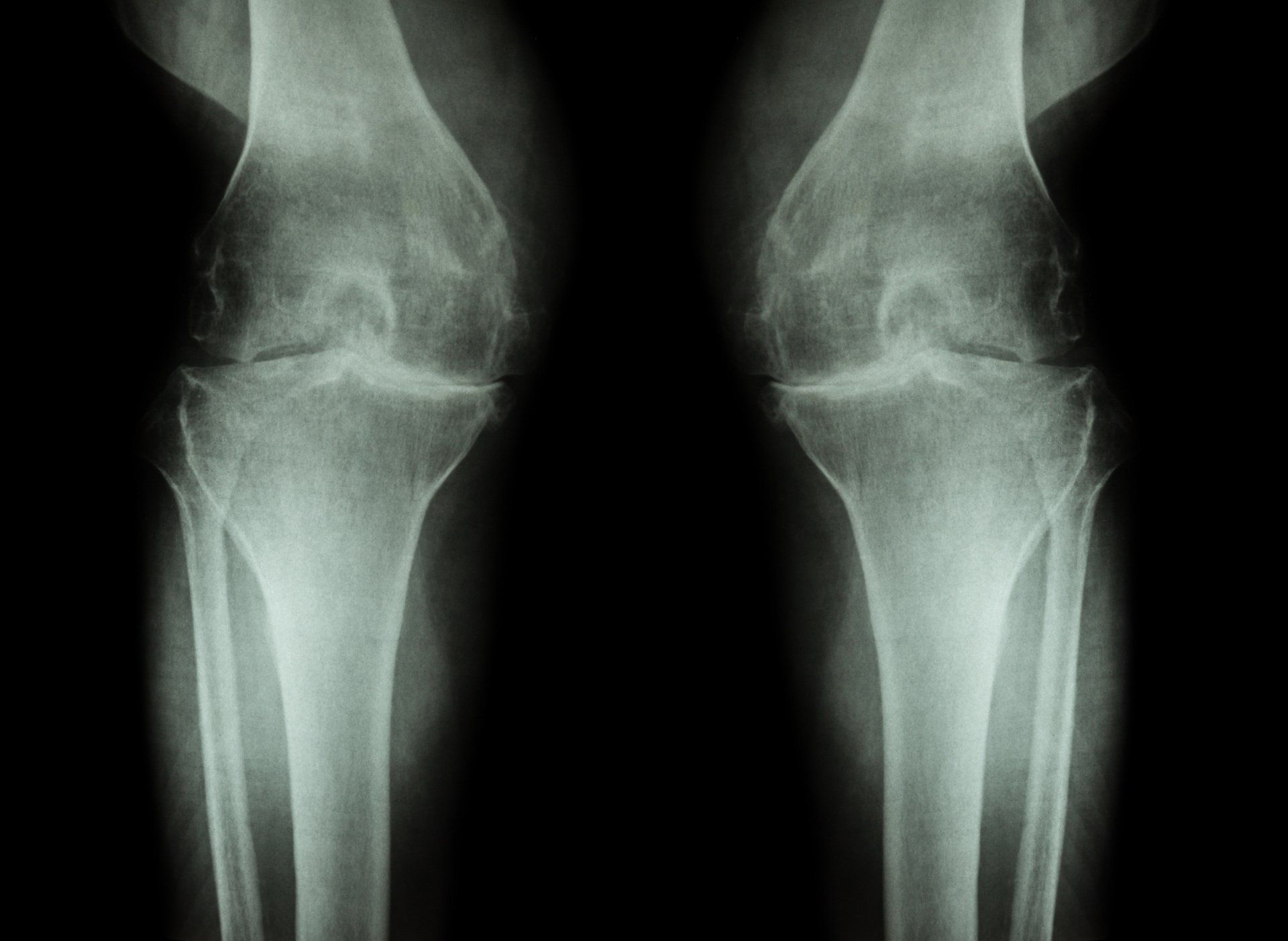
- X-rays are taken to confirm the diagnosis and they should be with the patient weight bearing so as to better detect the degree of joint space narrowing which is one of the key features of arthritis
- MRI scans may also be required, more so in less advanced cases and in younger patients, to better assess location and extent of the arthritis
Treatment
- The treatment of knee arthritis needs to be tailored to each individual patient, the severity of their symptoms, the impact on their activities of daily living, how advanced the arthritis is, the patient’s expectations and physical demands, and physiological age
- In general, it would always be advisable to try a period of conservative (non-surgical) treatment options which are safer, easier, and less invasive
- Treatment is then escalated according to how the patient responds, and their willingness to opt for more invasive interventions
Conservative (Non-surgical) Treatment Options
- Lifestyle changes and avoiding aggravating activities
- Rest during acute exacerbations
- Painkillers
- Losing weight through:
- Dieting
- Exercise:
- avoid high impact activities such as running
- focus on low impact activities such as cycling, cross-trainer, rowing, swimming
- Physiotherapy
- Offloading Knee brace: can be useful if arthritis affects one side of the knee and they serve to offload that compartment
- Walking aids
- Knee injections:
- Steroid: to reduce inflammation
- Hyaluronic acid: top up lubricant
Operative
- Knee arthroscopy in selected cases:
- Typically reserved for patients with mechanical symptoms of locking or sharp pain on twisting that haven’t settled after a period of rest
- High tibial osteotomy:
- Involves realigning the shin bone (tibia) to make it straighter and taking pressure off the worn-out painful part of the knee
- Suitable when:
- arthritis is isolated on one side of the knee (inner or outer half)
- Young (<50y) active healthy patients
- Not suitable if:
- Obese
- heavy smokers
- Poor vascular supply to legs
- marked stiffness
- inflammatory arthritis
- Unicompartmental knee replacement:
- This is a partial knee replacement of either the:
- Medial (inner) half of the knee – most common
- Lateral (outer) half of the knee - uncommon
- Involves resurfacing the affected half of the tibia and femur with metal and putting a plastic bearing in between
- Patellofemoral replacement:
- Suitable when patients have isolated advanced arthritis in the patellofemoral compartment of the knee i.e. where the patella glides on the femur called the trochlea:
- Often there is a history of:
- Patella instability
- Patella fracture
- Malalignment of the leg
- Abnormally shaped trochlea from birth (the part of the femur that the patella glides on)
- Total Knee Replacement:
- Suitable when there is:
- Widespread symptomatic arthritis in the knee
- Failed non-surgical treatment options
- Involves replacing the worn-out joint surface of the knee with metal above and below, and plastic in between