Introduction to the Knee Joint
Knee Anatomy
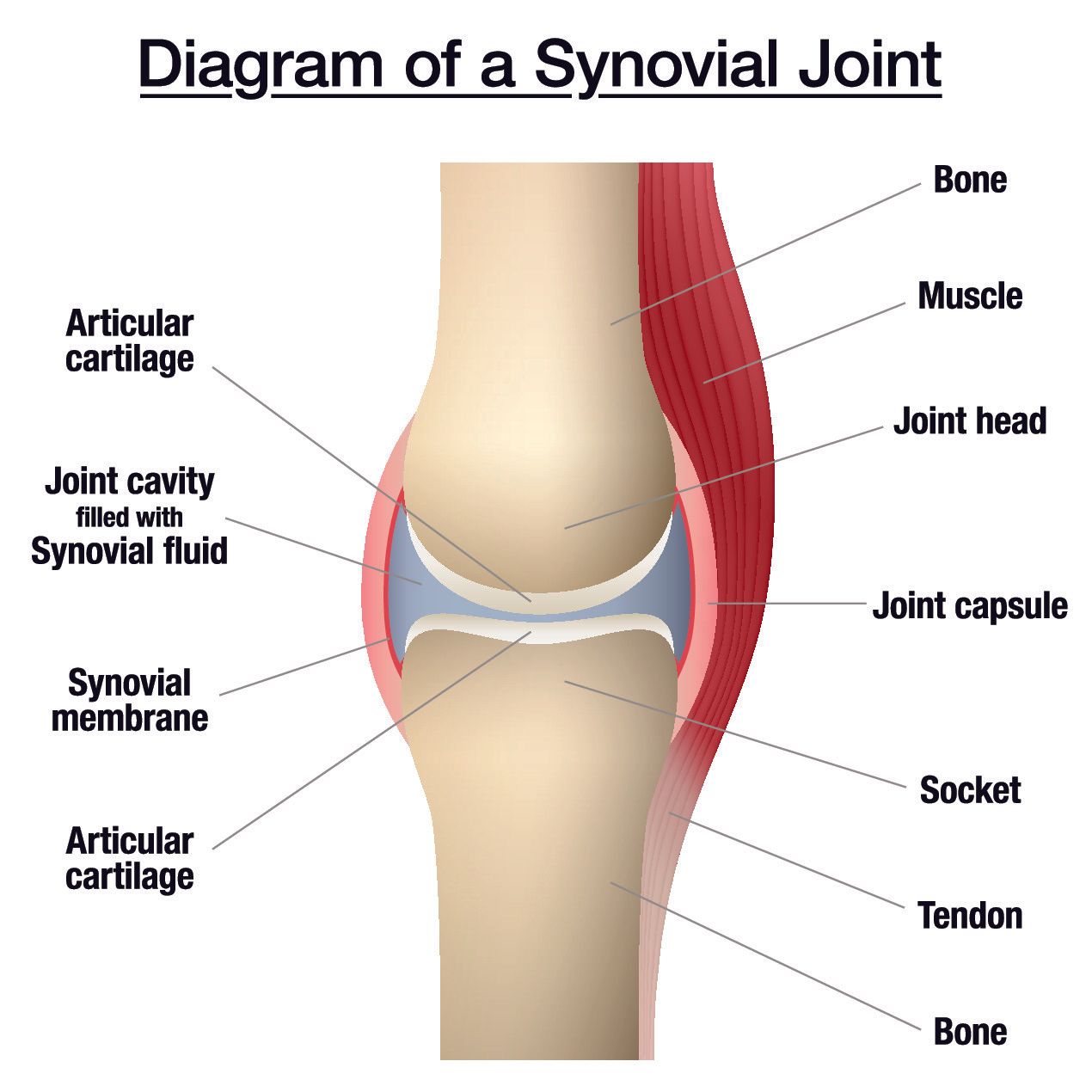
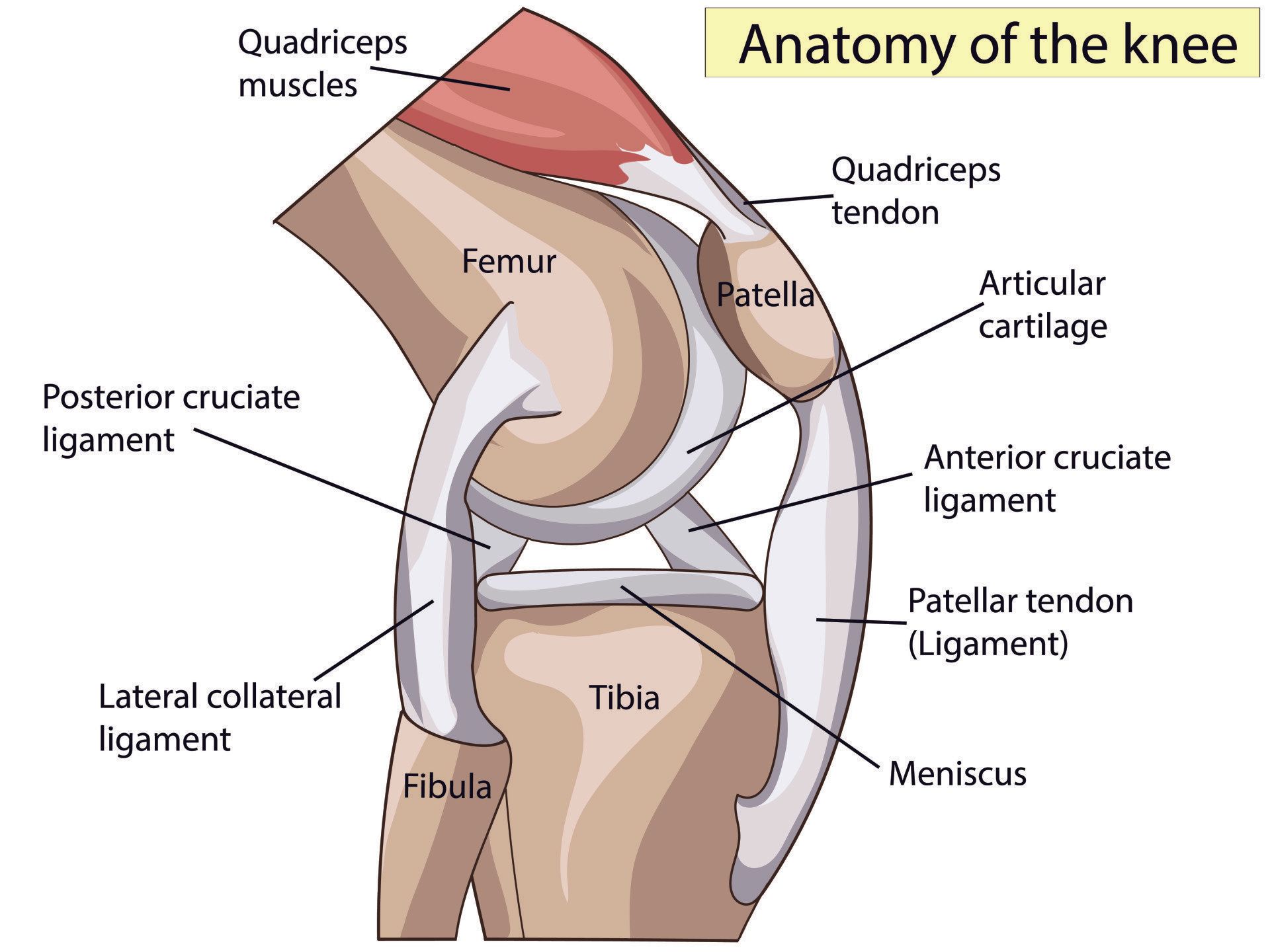
- The knee joint is a large synovial joint
- It is a complex hinge joint
- The main movements are:
- flexion (bending)
- extension (straightening)
- The following secondary movements occur but are more restricted:
- medial (internal) rotation
- lateral (external) rotation
- Knee motion is dependent on:
- action of muscles around the knee
- shape of the articular surfaces
- ligaments in and around the knee
- Like other synovial joints:
- bones are covered by articular (also known as hyaline) cartilage which minimises friction on movement
- the lubricant inside the joint is called synovial fluid
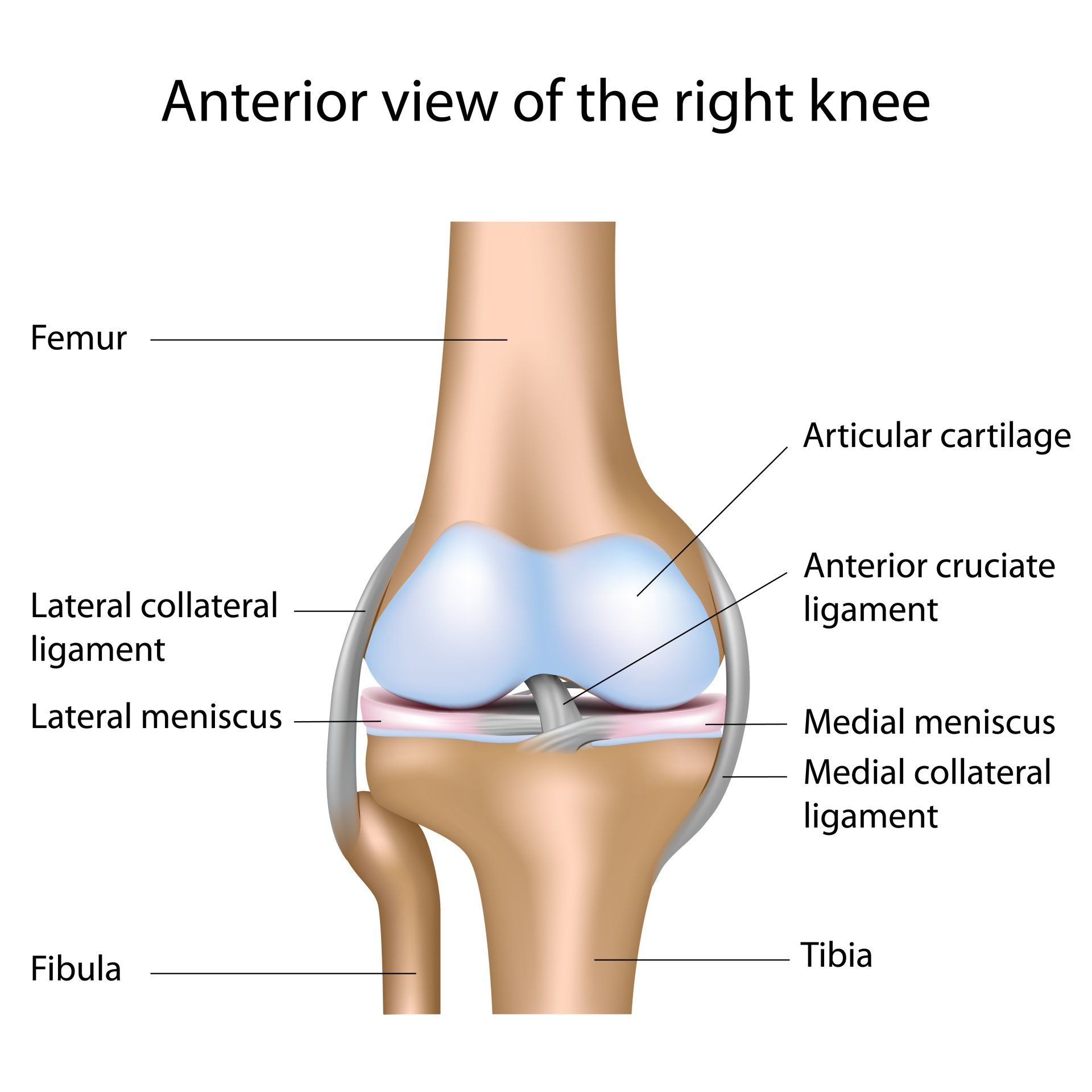
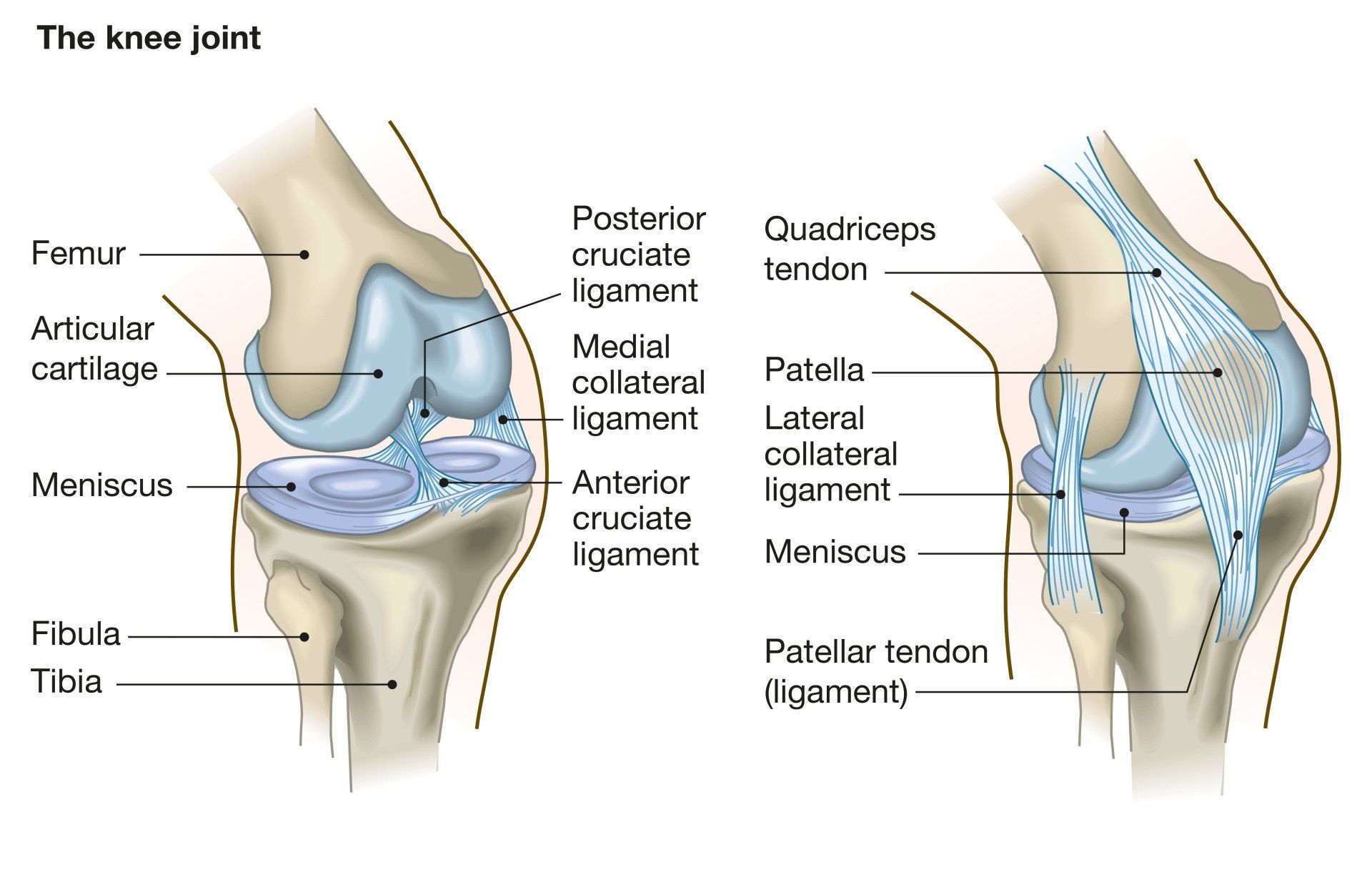
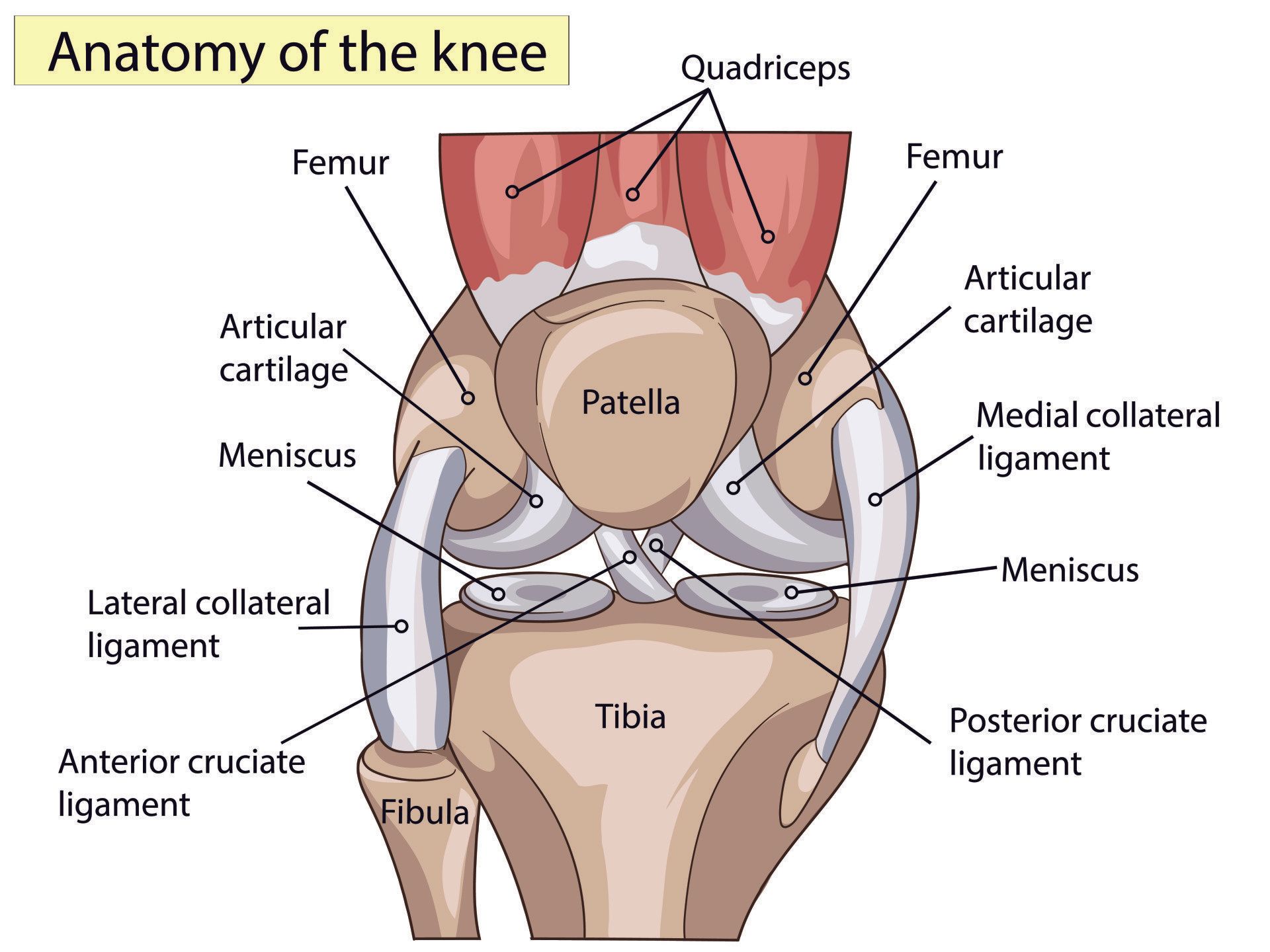
- The bones that form the knee joint are:
- Femur (thigh bone): the strongest and longest bone in the human body
- Tibia (shin bone): the primary weight bearing bone of the lower leg
- Patella (knee cap): sits at the front of the knee connecting the quadriceps muscle to the tibia
- The fibula is a smaller bone that runs parallel on the outside part of the tibia:
- whilst it does not form part of the articulation of the knee joint, it provides attachment to essential soft tissue elements of the knee joint such as the lateral (outer) collateral ligament
Joint surfaces
- The knee joint anatomically consists of two articulations:
- Tibiofemoral:
- between the medial and lateral femoral condyles above (proximally) and
- the medial and lateral tibial plateaus below (distally)
- on X-rays this is evaluated easier on the AP films
- Patellofemoral:
- between the patella (knee cap) anteriorly (at the front) and
- the trochlea part of the femur posteriorly (behind)
- on X-rays this is best evaluated on the lateral and skyline views
- Functionally orthopaedic surgeons split the knee into three compartments as each can often be dealt with in isolation:
- Medial tibiofemoral compartment
- Lateral tibiofemoral compartment
- Patellofemoral compartment
- When arthritis for instance is isolated in one of these three compartments they can be resurfaced in isolation whilst leaving the other two compartments intact
Patella and Patellofemoral Joint
- The patella (kneecap) is the largest sesamoid bone in the body
- Sesamoid bones like the patella are bones that are embedded within a tendon or muscle and they serve to reduce the friction on the tendon as it slides over a bony prominence
- Has the thickest articular cartilage in the body
- The patella by its nature as a bony prominence helps protect the front of the knee
- It also helps centralise the quadriceps tendon for optimal function
- The patella connects the quadriceps muscle via the quadriceps tendon to the tibial tubercle via the patella tendon
- It acts like a mechanical lever and by placing the quadriceps further away from the centre of rotation of the knee it helps amplify the pull of the quadriceps muscle by 30-40%
- Hence why removing of the patella (patellectomy) that was performed in the past for patellofemoral arthritis had poor results
- The patella articulates with the femoral trochlea forming the patellofemoral joint
- As the knee bends and straightens the patella glides up and down the femoral trochlea
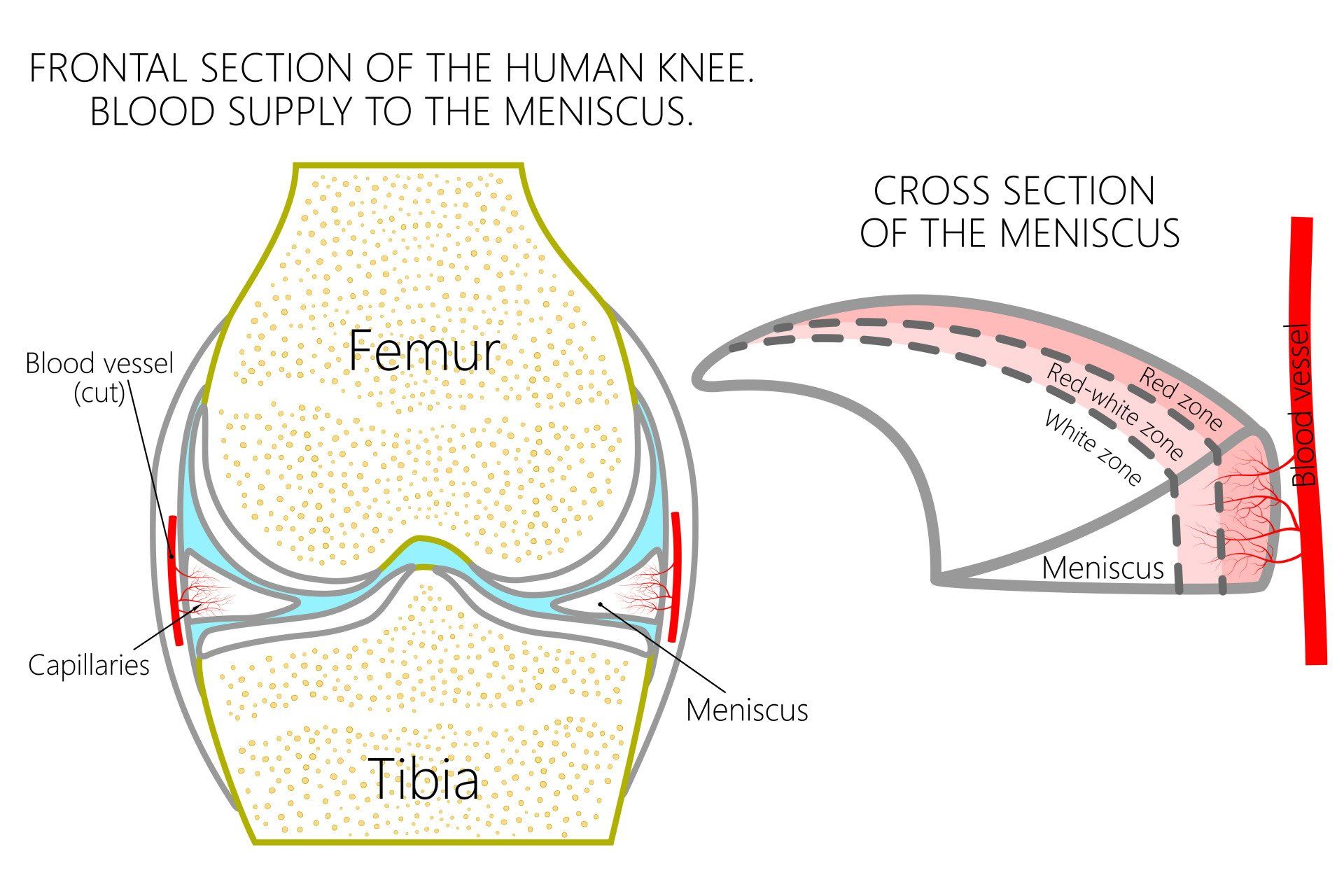
Articular cartilage
- The surface of the bones that form part of the knee joint is lined with articular cartilage which is a smooth white cushion covering the ends of the bones
- It can be easily seen when opening a joint of a chicken leg
- Whilst only a few millimetres thick, its function is to allow smooth movement to occur by reducing friction and therefore wear and tear
- It has the lowest coefficient of friction known to man (0.002) and it is 10 times more slippery than any engineered product
- It means that any load on the knee produces 1/500th of its value in friction
- It is composed of:
- water (~75%)
- proteins (primarily type II collagen)
- cells called chondrocytes
- Retention of water is critical to its mechanical properties and when there is wear and tear the ability to retain water is lost making it weaker and less protective
- Has no blood supply and so once damaged it cannot heal by itself
- It relies on diffusion of oxygen and nutrition to enter its cells from the surrounding synovial fluid which also helps lubricate the joint
- Has no nerve supply but when damaged, the underlying bone is subjected to increased stresses and as it is has nerve supply it manifests as pain
Meniscus
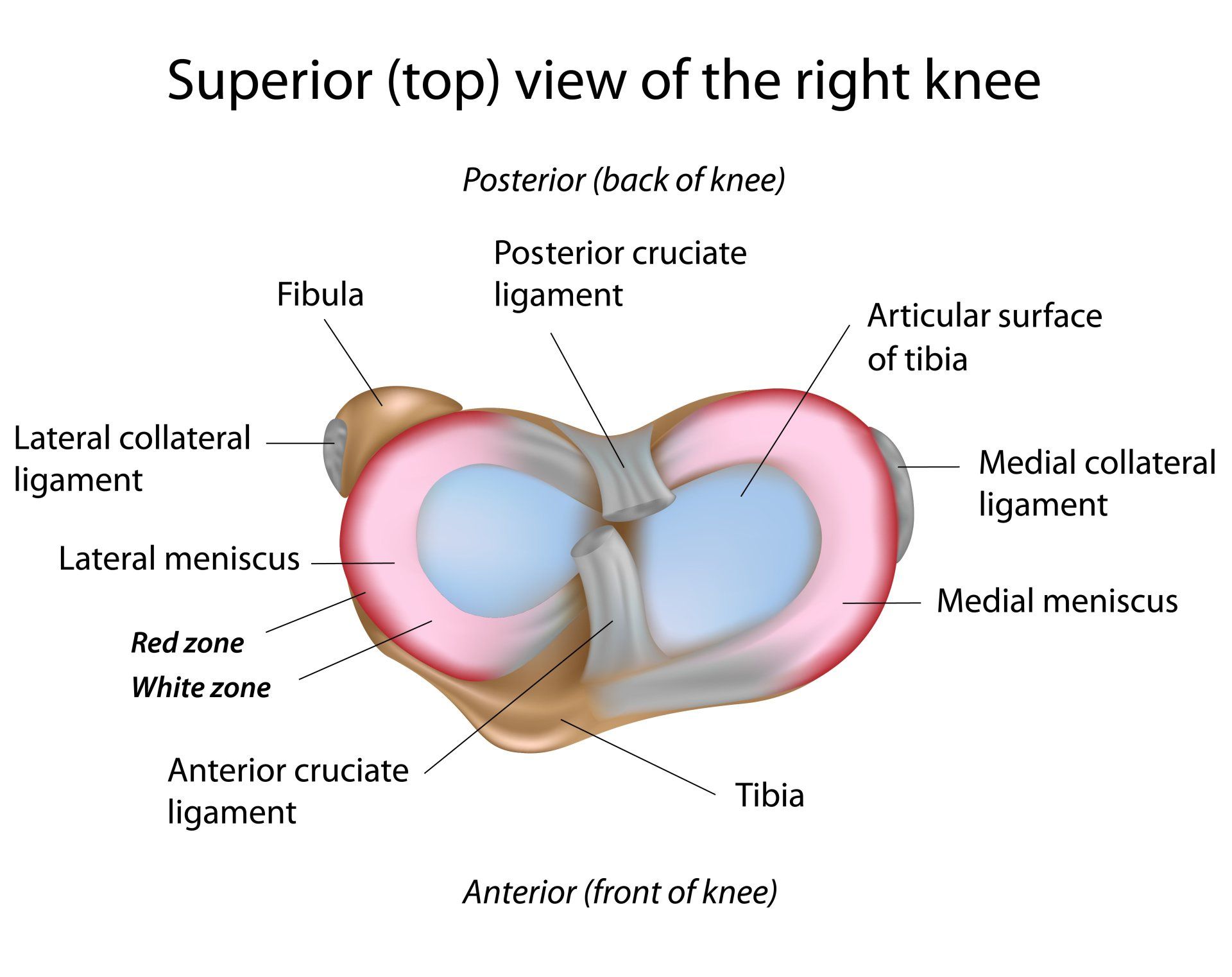
- The knee joint has two menisci:
- Medial (inner) meniscus:
- Covers a smaller portion (~60%) of the underlying tibial plateau
- It is more firmly attached than the lateral meniscus to surrounding tissues (medial collateral ligament and joint capsule)
- As a result is more commonly injured overall than the lateral meniscus
- More commonly injured in chronic ACL tears
- Lateral (outer) meniscus:
- Covers a larger portion (~85%) of the underlying tibial plateau
- Is less adherent to surrounding tissues, is not attached to the lateral collateral ligament and so is much more mobile
- Therefore is less commonly injured overall than the medial meniscus
- More commonly injured than medial meniscus in acute ACL tear
- Like articular cartilage they are a type of cartilage called fibrocartilage
- Meniscus is more rubbery and less spongy than articular cartilage
- They are C-shaped and are located between the articular surfaces of the femur and tibia
- Medial meniscus is more crescent shape
- Lateral meniscus is more circular
- Descriptively they are split into thirds
- Anterior (front)
- Middle
- Posterior (back)
- The anterior and posterior thirds of each meniscus each has a horn which then anchors the meniscus into the bone via the meniscal root
- In other words, each meniscus is anchored to the bone (tibia) via the anterior (front) and posterior (back) meniscal roots
- If these meniscal roots (anchors to the bone) are torn then the whole meniscus is defunctioned and they lose their protective function
- Meniscal root tears are increasingly recognised but require more complex techniques to repair them
- The two menisci are connected at the front via the transverse intermeniscal ligament
- Discoid meniscus:
- Is a disc shaped meniscus rather than C-shaped, it is thicker and covers a greater area of the underlying bone than normal
- It is a normal variant occurring about 3-5% of the population
- It is a congenital anomaly meaning the person was born with it
- Typically affects the lateral meniscus
- Found bilaterally (in both knees) in ~20%
- If asymptomatic should be left alone
- They are more prone to tearing than normal meniscus:
- If this becomes symptomatic then the meniscus is trimmed to a more normal C shape
- Their function is to:
- Act as shock absorbers
- Medial meniscus: takes 50% of the load going through the medial half of the joint when the knee is fully straight and 85% when the knee is flexed at 90 degrees
- Lateral meniscus: takes 70% of the load going through the lateral half of the joint when the knee is fully straight and 85% when the knee is flexed at 90 degrees
- Deepen the articular surfaces thus spreading the load over a larger contact surface area and reduce stress on the articular cartilage
- Increase stability of the knee joint:
- The meniscus cups the femur so it provides additional front to back stability (especially the medial meniscus)
- Tear of the posterior root of the medial meniscus in the presence of ACL injury adds to the antero-posterior (front to back) instability of the knee and failure to repair both, compromises the outcome on knee stability
- Tear of the posterior root of the lateral meniscus adds to the rotational instability of the knee
- Aid lubrication of knee joint:
- Meniscus acts like a windscreen wiper spreading synovial fluid over the articular cartilage
- Aid nutrition of articular cartilage:
- By spreading the synovial fluid over the articular cartilage, it assists in providing nutrition
- The blood supply to the meniscus comes from its attachment peripherally to the joint capsule and can be broken down into thirds:
- Outer peripheral third (red zone): has good blood supply and good healing potential
- Middle third (red-white zone): sparse blood supply meaning little healing potential
- Inner third (white-white zone): no blood supply, reliant on diffusion only, so no healing potential
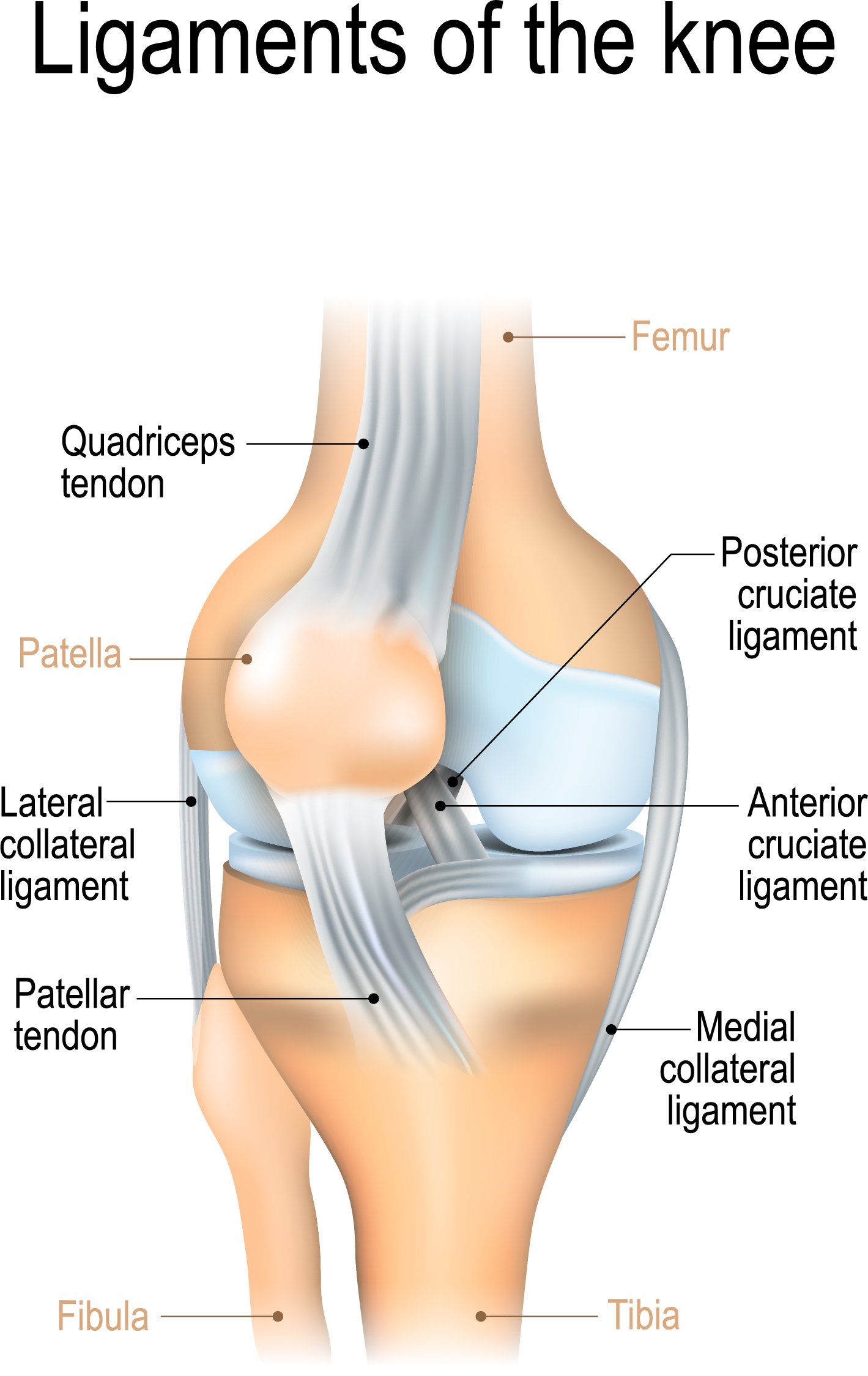
Ligaments around the knee
- The main ligaments around the knee are the:
- Medial (inner) and Lateral (outer) collateral ligaments
- Anterior (front) and Posterior (back) cruciate ligaments
- The collateral ligaments are located in the periphery and are outside the capsule (lining) of the knee joint:
- Medial Collateral Ligament (MCL):
- Located on the inner side of the knee connecting the femur with the tibia and helps to resist valgus forces to the knee i.e. foot forced further away from the midline in relation to the knee
- Lateral Collateral Ligament (LCL):
- Located on the outer side of the knee connecting the femur with the fibula head and helps to resist varus forces to the knee i.e. foot forced towards the midline in relation to the knee
- The cruciate ligaments (ACL and PCL) on the other hand are intracapsular and are located in the middle of the knee and as their name suggests they cross each other:
- Anterior Cruciate Ligament (ACL):
- Attaches from the front central part of the tibia to the lateral (outer) femoral condyle at the back
- It helps prevent the tibia moving forward (anterior) in relation to the femur as well as provide rotational stability
- Posterior Cruciate Ligament (PCL):
- Attaches from the back of the tibia to the medial (inner) femoral condyle at the front
- It helps prevent the tibia moving backwards (posterior) in relation to the femur
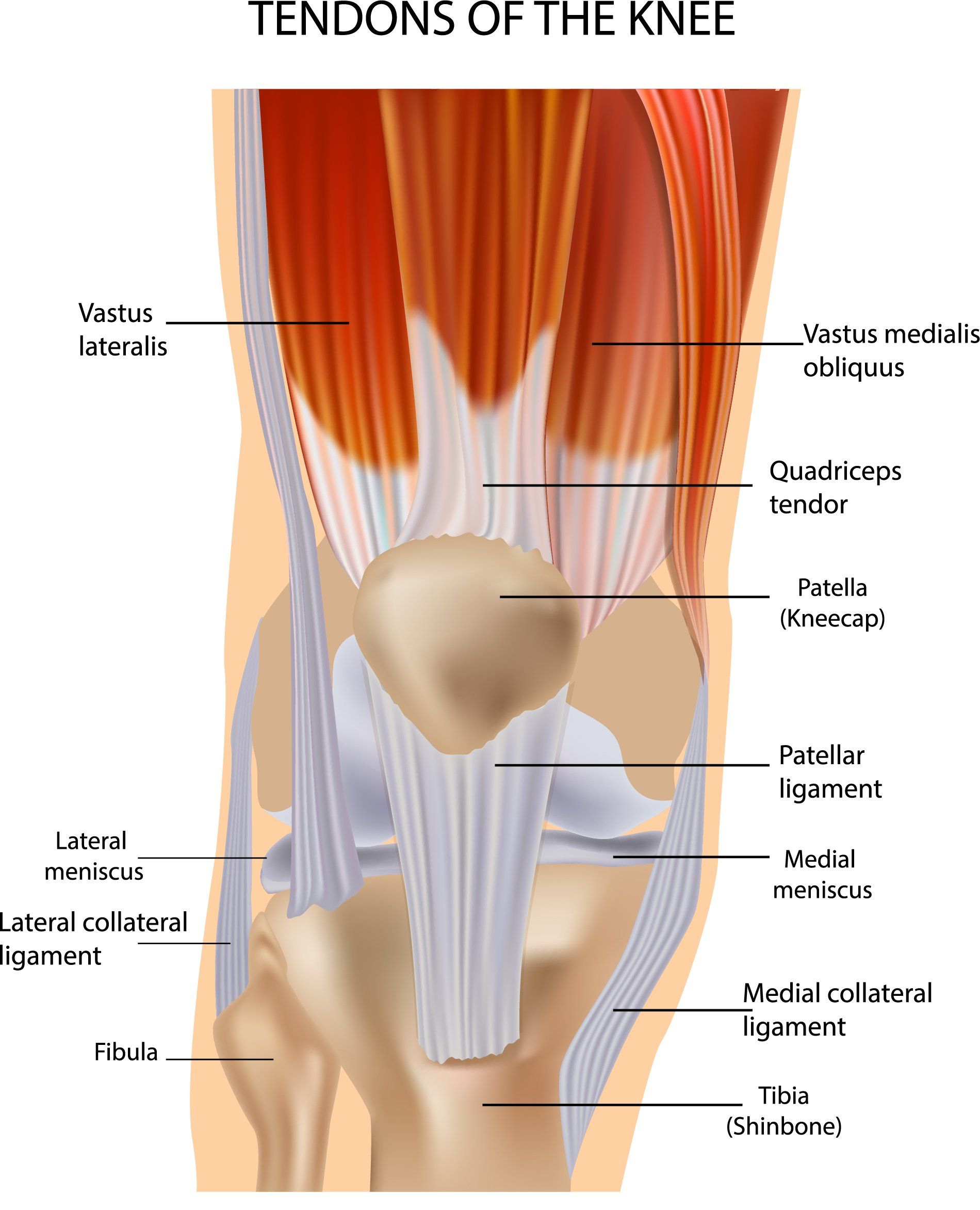
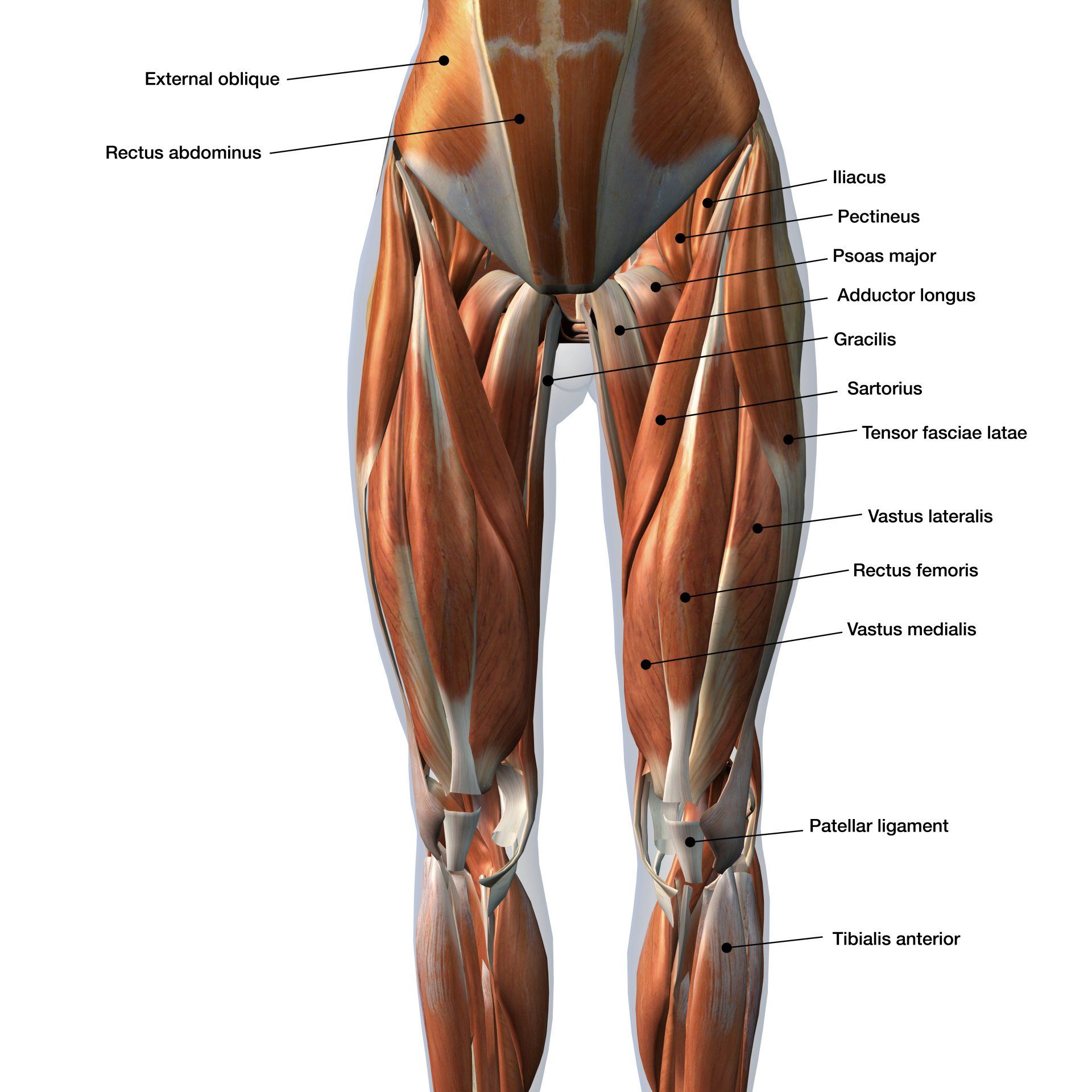
Muscles and Tendons around the Knee
- The tendons around the knee can be grouped by those serving:
- anterior (front) thigh muscles called quadriceps femoris
- the posterior (back) thigh muscles called hamstrings
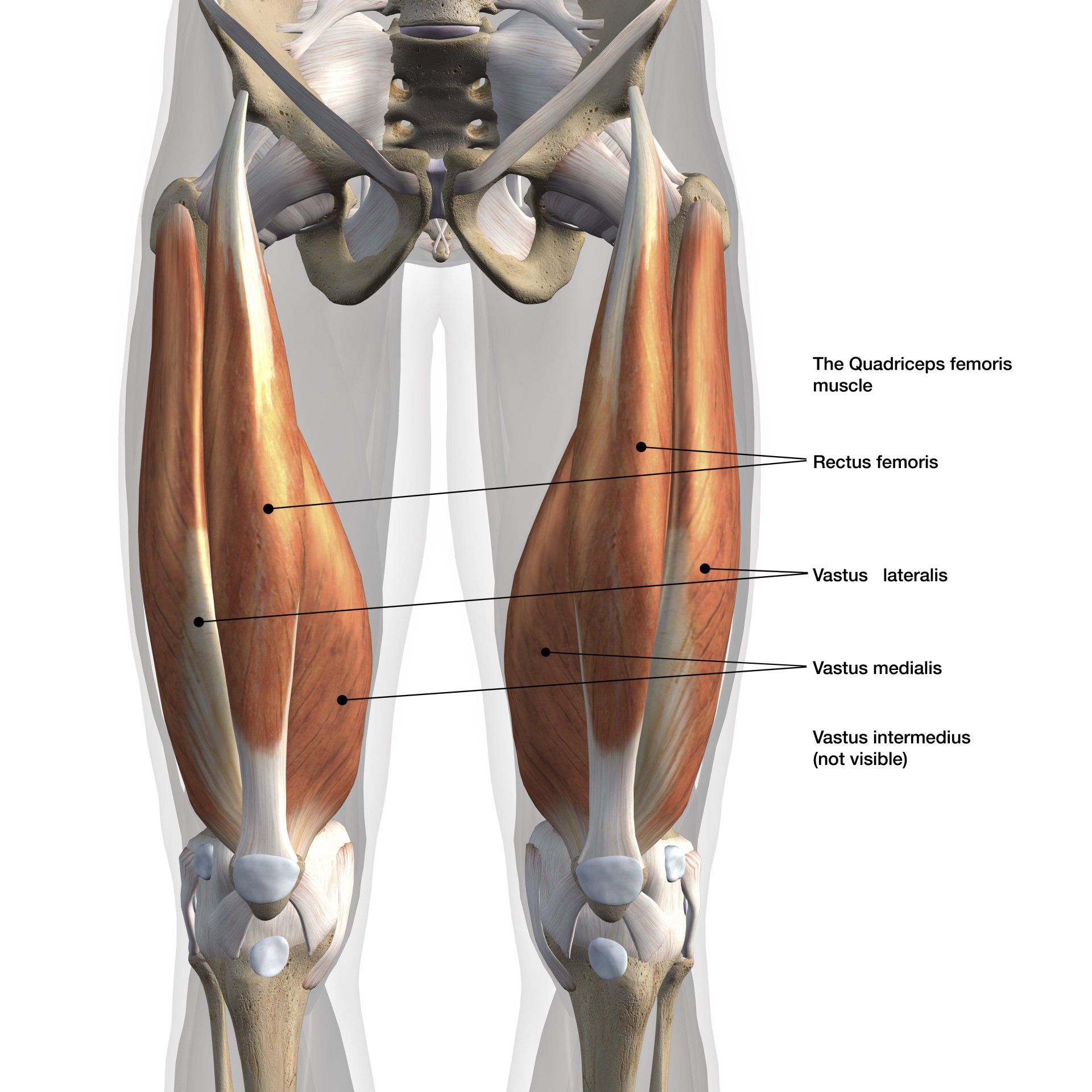
- The quadriceps femoris muscle is composed of a group of 4 muscles called:
- Rectus femoris
- Located anteriorly (at the front)
- Vastus medialis
- Located on the medial (inner) side of the femur
- Vastus lateralis
- Located on the lateral (outer) side of the femur
- Vastus intermedius
- Located between vastus lateralis and vastus medialis but deep to rectus femoris
- The function of the quadriceps femoris is to extend the knee:
- It is a powerful extensor of the knee
- However it is the only muscle that extends the knee and if it is injured (particularly its two tendons) can cause major disability
- There are two tendons that relate to the quadriceps muscle and form part of the extensor mechanism:
- Quadriceps tendon:
- Provides insertion of the quadriceps muscle to the patella (knee cap)
- Patella tendon:
- Connects the patella to the tibial tubercle (bony prominence at the front of the tibia few centimetres below the knee joint level)
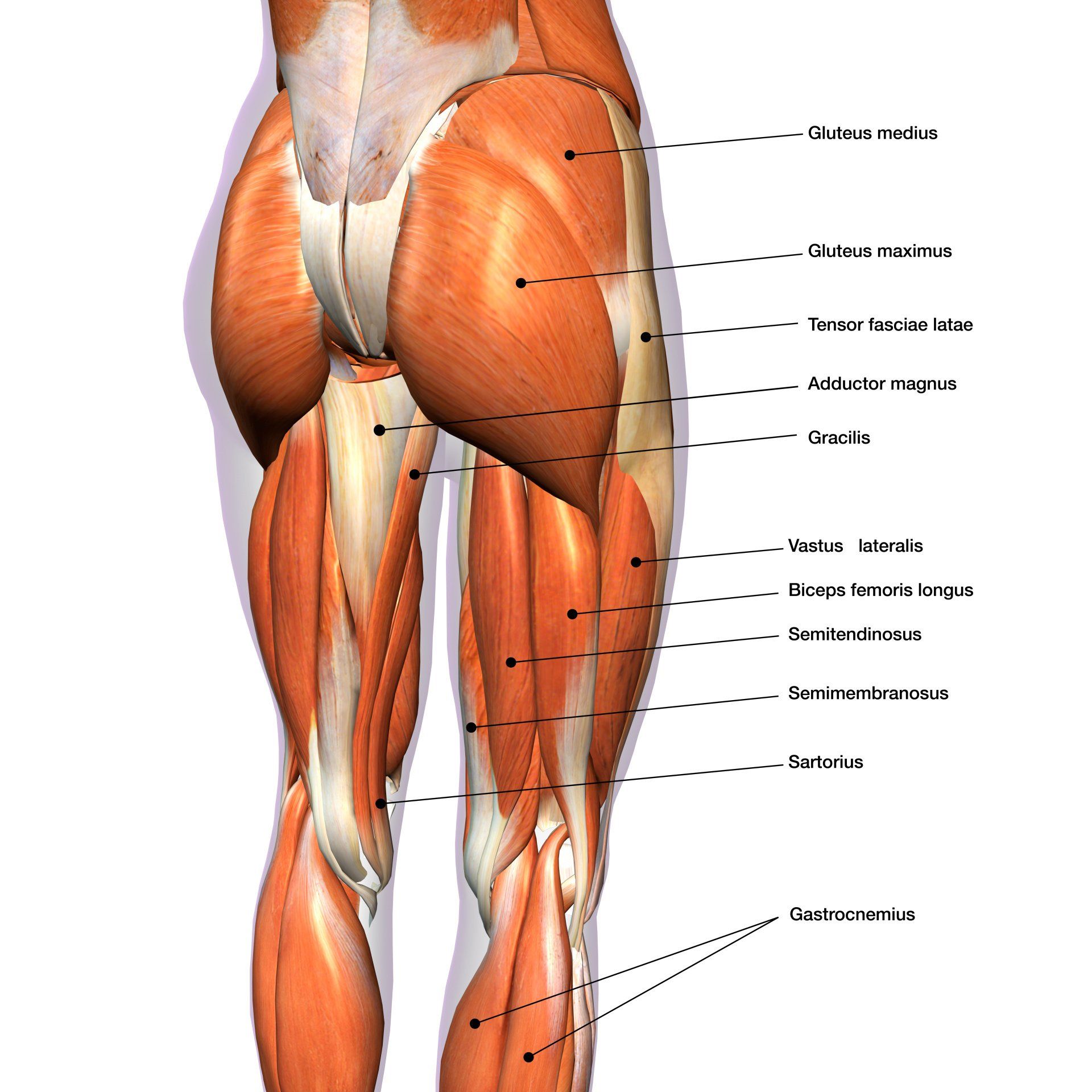
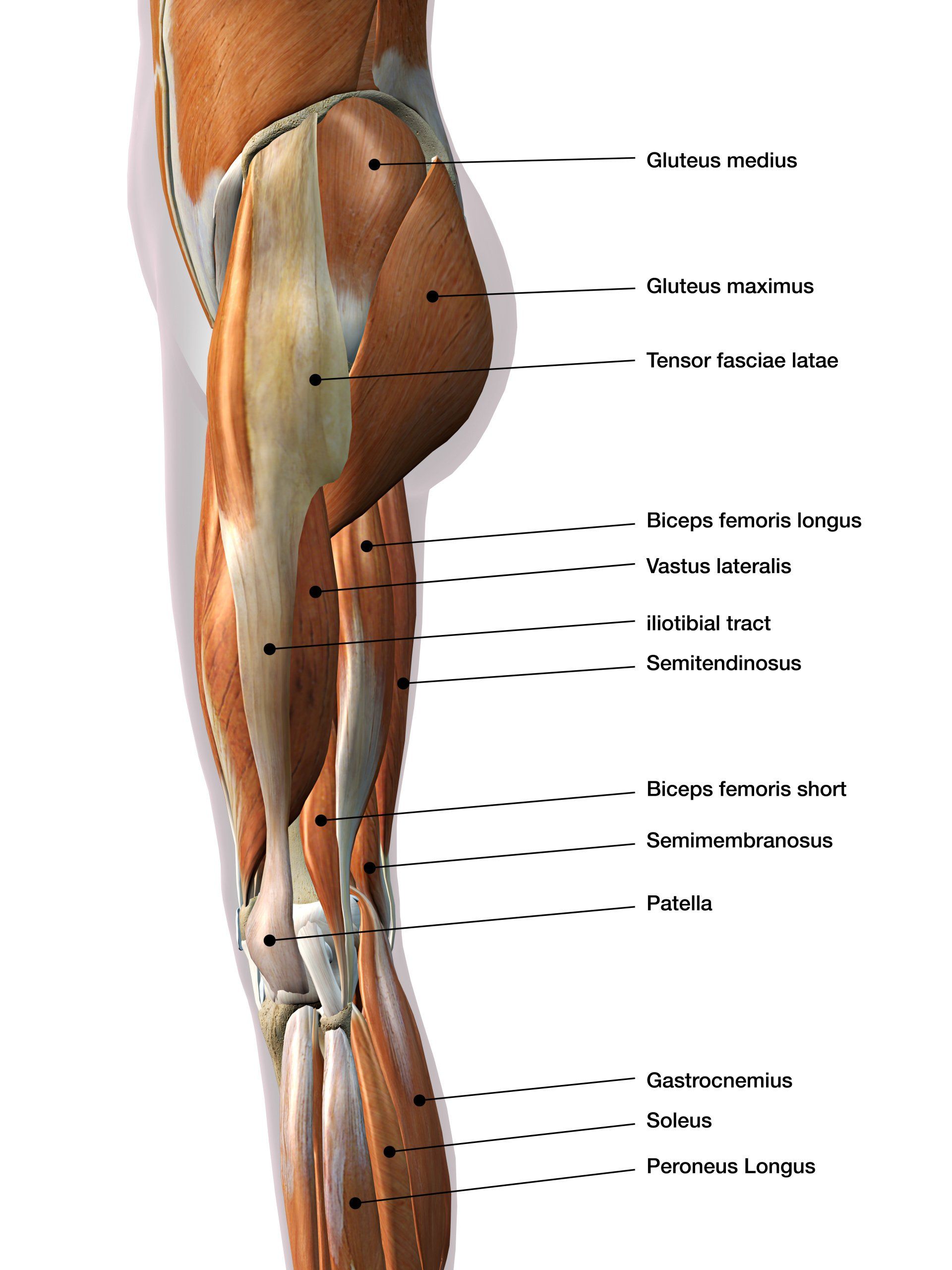
- Hamstrings are a group of three muscles at the back of the thigh and are comprised of:
- Semimembranosus:
- It is a flat tendon and the most medial of the three hamstring tendons
- It originates from the ischial tuberosity and inserts into the medial tibial condyle
- It functions to extend the hip, flex the knee and internally rotate the tibia when the knee flexes
- Semitendinosus:
- It originates from the ischial tuberosity and inserts into the pes anserinus part of the proximal tibia
- It functions to extend the hip, flex the knee and internally rotate the tibia when the knee flexes
- Biceps femoris:
- It originates from the ischial tuberosity and inserts into the fibular head
- It functions to extend the hip, flex the knee and externally rotate the knee
- Hamstrings originate above the hip joint at the ischial tuberosity (bony prominence of the pelvis that you sit on) and attach below the knee joint line
- Their function is to flex the knee and extend the hip
- Since hamstrings cross over two joints (hip and knee) they are termed biarticular and are essential in complex functional movements and stability of the lower limb
- Tendons on the medial (inner) side are the sartorius, gracilis and semitendinosus:
- They insert on the proximal anteromedial side of the tibia called pes anserinus in the order stated from proximal to distal
- Gracilis and semitendinosus are two commonly harvested tendons for ligament reconstructions around the knee
- Semimembranosus forms part of the hamstring muscles
- Tendons on the lateral (outer) side:
- Biceps femoris is another hamstring tendon and it inserts on the fibular head
- Popliteus tendon is not part of the hamstring complex and is the only tendon that pierces the joint capsule (it is described further in the posterolateral corner section)
Anterior Cruciate Ligament (ACL)
- One of the four major ligaments in the knee
- Located in the middle of the knee called the intercondylar notch
- Measures 33x11mm
- Load to failure of 2200 Newtons
- ACL arises on top of the tibia towards the front and passes superiorly (upwards), posteriorly (backwards) and laterally (outwards)
- It attaches to the medial (inside) wall of the lateral (outer) femoral condyle
- ACL prevents the tibia moving excessively anteriorly (forward) in relation to the femur as well as provide rotational stability especially when the tibia rotates externally (outwardly) in relation to the femur
- Hence it is essential in activities that involve changing direction
- Classic method of injury is a non-contact twisting valgus injury on a loaded and flexed (bent) knee and the tibia internally rotates in relation to the femur
- The ACL is comprised of two bundles: anteromedial and posterolateral bundles
- Patient’s feeling of instability and confirmation of a lax/defunctioned ACL on examination help guide need for surgery when suspect partial ACL tear
Posterior Cruciate Ligament (PCL)
- The posterior cruciate ligament (PCL) is the other cruciate ligament and is also located in the middle of the knee (intercondylar notch)
- PCL crosses in the middle of the knee in the opposite direction to the ACL
- PCL arises from the back of the tibia and passes superiorly (upwards), anteriorly (forewords), and medially (inwards)
- It attaches on the lateral (outer) side of the medial (inner) femoral condyle
- Measures 38x13mm
- Load to failure of 2500 Newtons
- Therefore, it is a larger and stronger ligament than the ACL
- It is far less commonly injured than the ACL
- Its function is to help prevent the tibia going backwards in relation to the femur
- Classic method of injury is a backwards directed force on the tibia such as hitting the tibia on the dashboard in a road traffic collision or landing directly on the tibia with the knee bent during a fall
Medial Collateral Ligament (MCL)
- Medial Collateral Ligament (MCL) is located on the inside part of the knee
- MCL arises close to the medial femoral epicondyle and attaches to the inner side of the tibia over a wide area
- It functions to resist valgus force i.e. the foot going away from the midline in relation to the knee (knock kneed position)
- It has two components:
- Deep MCL:
- Sits next to the knee joint and attaches over a short distance
- Attaches to the medial meniscus
- It is the weaker of the two components
- Superficial MCL:
- Is further away from the knee joint than the deep MCL
- Is the primary stabiliser to valgus force in the knee
- Unlike the LCL it is quite a flat and broad structure
- Despite having a strength of 4000 Newtons, it is the most commonly injured knee ligament
- But has a good bloody supply and heals well with bracing
Lateral Collateral Ligament (LCL)
- Lateral collateral ligament (LCL) is located on the outside part of the knee
- LCL connects outside part of femur (lateral femoral epicondyle) to the fibular head
- Its function is to resist varus i.e. the foot going towards the midline in relation to the knee (bow legged position)
- It is a cord like structure, much thinner, smaller and weaker than the MCL
- Load to failure of only 750 Newtons
- Despite being the weakest of the major knee ligaments, it is the least commonly injured ligament
- LCL injury often occurs in association with other injuries such as to the Posterolateral Corner (PLC) or Posterior Cruciate Ligament (PCL)
- It has poor blood supply and rarely heals with just bracing unlike MCL
Posterolateral Corner (PLC)
- The posterolateral corner is the corner of the knee located towards the back and outside part of the knee
- It comprises of numerous structures (i.e. not a single structure) and the three most important ones are:
- Lateral collateral ligament (LCL): as detailed above
- The popliteus tendon:
- This is the tendinous part of the popliteus muscle
- The popliteus muscle arises from the outer aspect of the lateral femoral condyle of the femur and inserts at the back of the tibia a bit below the knee joint
- The popliteus tendon pierces the joint capsule (lining) but is not within synovium
- It sits next to the lateral meniscus towards the back but it is not attached to it
- The popliteofibular ligament:
- this is a small ligament that connect the popliteus tendon to the fibula head
- The function of the posterolateral corner is to prevent excessive external rotation of the tibia in relation to the femur
- Isolated PLC injuries are rare but most commonly seen in conjunction with other ligamentous injuries such as ACL or PCL
Bursae around the Knee
- A bursa is a fluid filled sac and it helps reduce friction between muscles, tendons, bones and ligaments
- They essentially help cushion the pressure points around the knee
- They can vary in number but usually around 14 exist around the knee
For more information on symptomatic bursae
click here
Plica
- Plica is a fold of synovium within the knee joint
- Thought to be remnant of embryonic connective tissue that failed to resorb during foetal development
- It is thought that plicae are present in about 50% of the population and their size is variable
- They are elastic, thin and pliable structures and almost transparent like a membrane
- There are four well documented plicae:
- Infrapatellar plica (also known as (ligamentum mucosum):
- Most common plica in the knee
- Located in middle of knee (intercondylar notch) going from patella fat pad to centre of notch
- Can sometimes be confused as the ACL
- Suprapatellar plica:
- Located in suprapatellar space (knee joint space proximal to patella)
- Extends from medial knee wall towards lateral wall
- Medial plica:
- Located on the medial wall of the knee
- Extends from infrapatellar fat pad medially around the medial femoral condyle and into the medial wall of the knee
- The most commonly irritated plica due to repeated abrasion over the medial femoral condyle as the knee flexes and extends
- Lateral plica:
- Located on the lateral side of the knee
- The rarest form and rarely causes symptoms
Knee Motion
- Movement in the knee can be considered very simplistically to be flexion (bending) and extension (straightening) as would happen with any hinge joint
- Reality though is very much more complicated and is a composite movement of:
- Flexion: bending
- Extension: straightening
- Rollback:
- As the knee flexes the femur slides posteriorly (backwards) on the tibia so as to clear it and allow greater flexion
- Rotation:
- In order for the knee to bend from its full extended position when standing, the popliteus unlocks the knee by externally rotating the femur on the tibia
- This is essential for rollback and flexion to occur
- Pivot:
- The medial compartment is very congruent i.e. the surfaces match and the medial femoral condyle is able to sit well inside the dished (concave: rounded inwards) medial tibial plateau
- As a result, during flexion there is minimal front to back sliding of the medial femoral condyle on the medial tibial plateau
- The lateral compartment is incongruent i.e. the surfaces don’t match as the lateral femoral condyle is convex (rounded outwards) so during flexion there is a lot more sliding of the lateral femoral condyle on the lateral tibial plateau which assists with the rollback mechanism
- Normal knee movement is therefore reliant on:
- Articular geometry (shape of the joint surfaces)
- Ligaments
- Muscles
- If any of these are affected then it will have an impact on knee movement and stability and consequent wear and tear and pain
- The four main movements that occur at the knee and the muscles producing these movements are:
- Extension: quadriceps muscle which through the quadriceps tendon inserts into the patella and then patella tendon into the tibial tuberosity
- Flexion: hamstrings, gracilis, sartorius, popliteus and plantaris
- Lateral/external rotation: biceps femoris
- Medial/internal rotation: semimembranosus, semitendinosus, gracilis, sartorius and popliteus