ACL Injury in Children
Why are ACL injuries continually increasing in children?
- The number of ACL injuries in children is rapidly rising:
- Number of children participating in sport is rising
- Children’s sports are increasingly competitive often with the incentive of financial reward in the future
Why ACL injuries in children are most concerning out of any age group?
- The consequences of an ACL injury in this age group is the most concerning out of any other population:
- It can compromise their quality of life
- Increase risk of further injury
- Propagate early knee arthritis
- ACL injuries in children carry a poor prognosis unless surgery is carried out because:
- It is extremely difficult to restrict children on their physical activities
- The recurrent knee instability episodes increase the risk of meniscal and articular cartilage damage and therefore subsequent early arthritis
- Within 10 years of ACL injury a child is likely to have:
- Meniscal tear (65%)
- Osteoarthritis (45%)
- Osteochondral fracture (15%)
- Girls have a 3-5 higher rate of ACL injuries than boys participating in the same sport
Why children should have an ACL reconstruction and not wait until they are adults?
- They should have ACL reconstructed promptly to prevent further injury inside the knee
- It is difficult for this age group to abstain from sporting activities
- Without an ACL, recurrent instability episodes occur that put at risk cartilage and menisci with disastrous consequences for rapid onset osteoarthritis
- Surgery should not be delayed by more than 5 months as this:
- Doubles the risk of requiring medial meniscal surgery
- Risk increases to 6 times if delayed by more than a year
What are the challenges in paediatric ACL reconstructions?
- Children are not just small adults
- There are numerous differences that make ACL reconstructions in children more complex than in adults
- They have skeletal and physiological differences that make them unique
- The key challenges are:
- Growth plates:
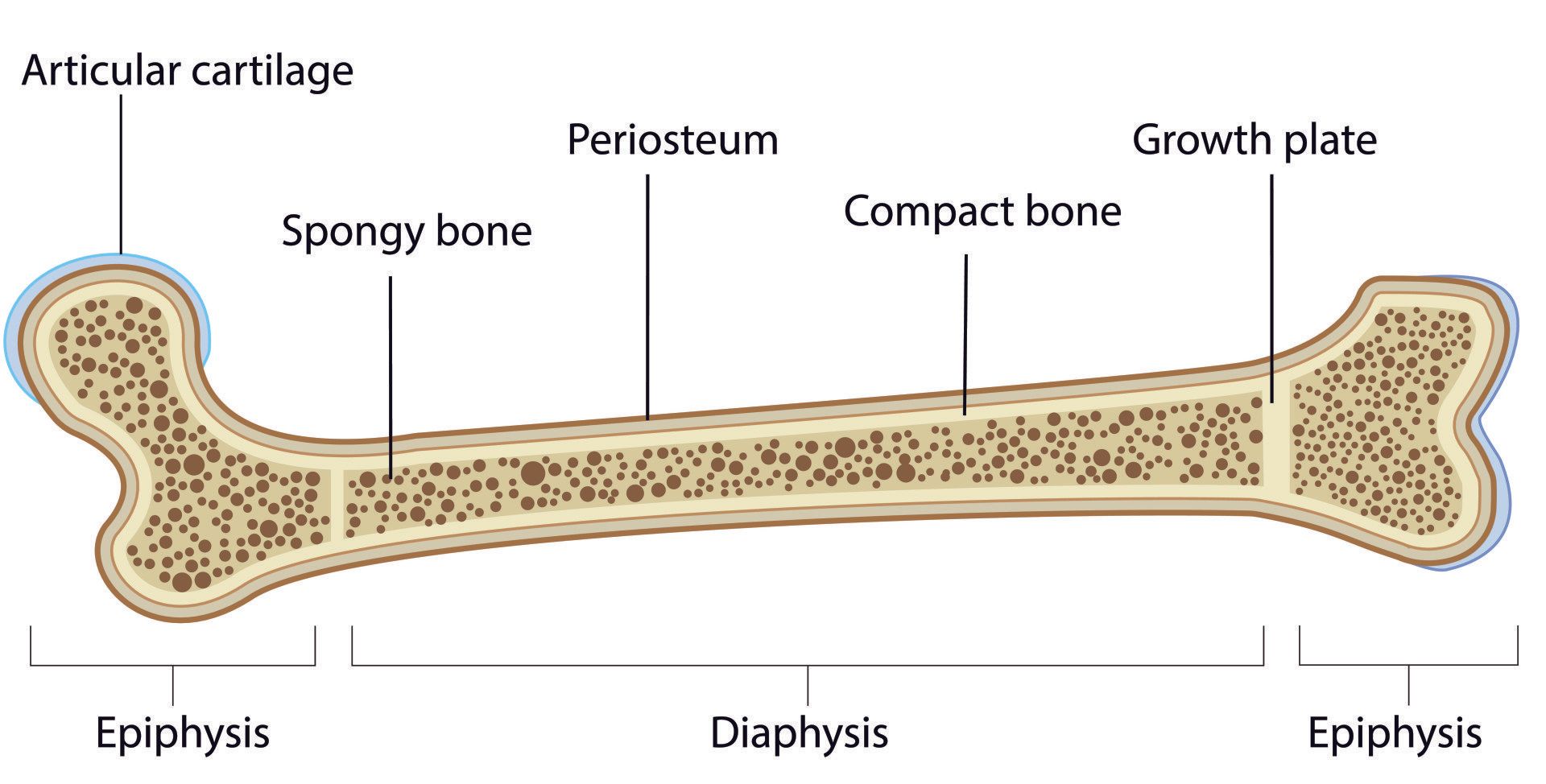
- Growth plate (also called physis) is the area of bone that allows it (and therefore the child) to grow in height
- Growth plates are present on either end of long bones (e.g. femur, tibia, humerus)
- Around the knee there are two growth plates:
- Distal femur (lower end of the thigh bone)
- Proximal tibia (upper end of shin bone)
- They are the softest and weakest part of a child’s growing skeleton as they lack calcium:
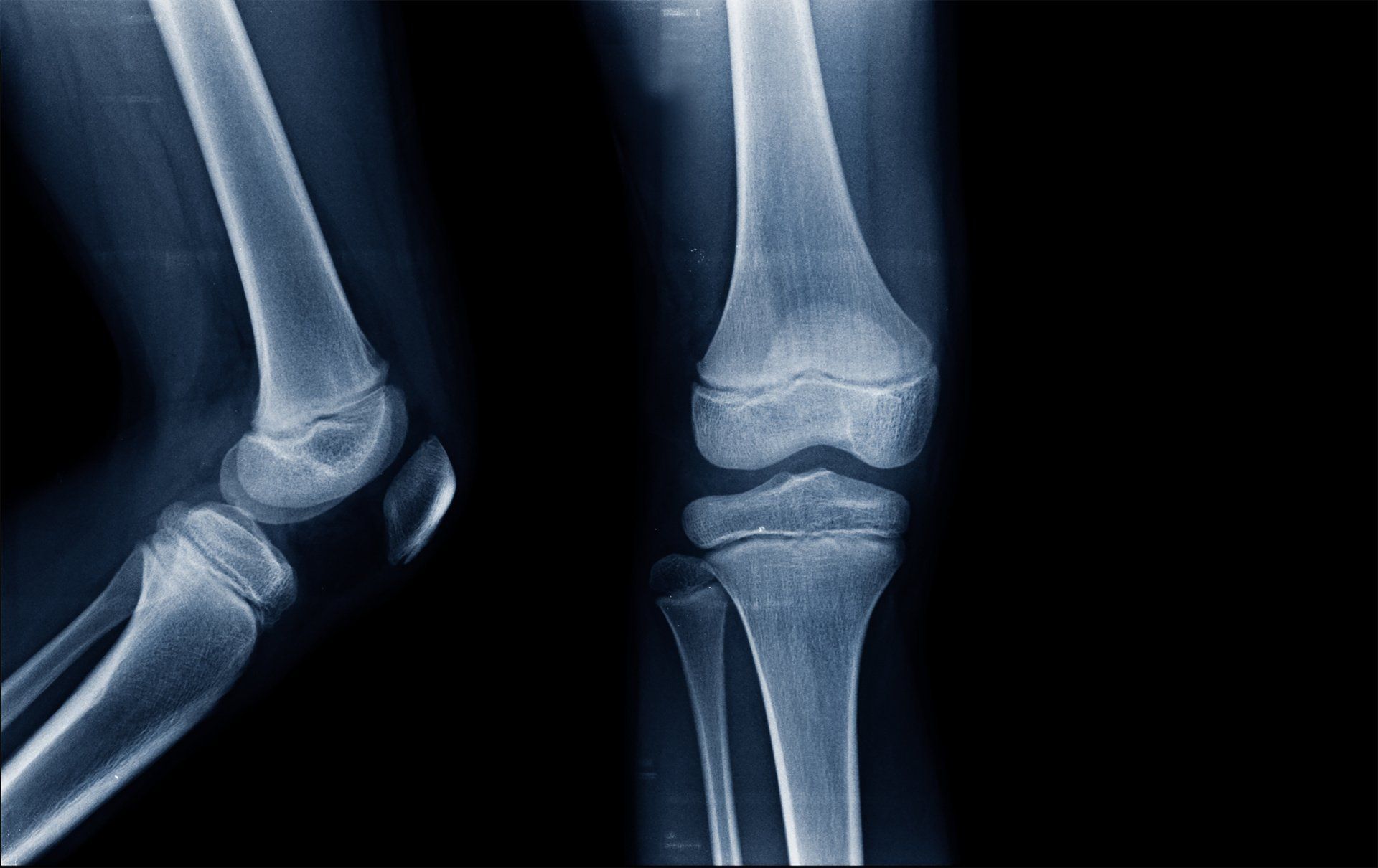
- As a result, they are seen on X-ray via the black line that crosses the bone parallel to the joint plane:
- presence of calcium is what makes bone appear white on X-ray so the lack of calcium in growth plates makes them look black
- During an ACL reconstruction bony tunnels are made in the femur and tibia for the graft to pass through:
- These tunnels can cause damage to the growth plates so the options are:
- to change the orientation of the tunnels to minimise the damage (which has been shown to be very effective) or
- to drill the tunnels to completely avoid the growth plates which unfortunately creates other problems
- No fixation devices, implants or bone blocks should cross the growth plate so as not to cause fusion across it and ultimately growth disturbance
- Restricted ACL graft options:
- Only soft tissue grafts should cross a growth plate:
- A bone block e.g. from a patella tendon graft would cause fusion of that part of the growth plate it traverses and lead to shortening and/or malalignment of the limb
- Synthetic grafts are not recommended due to damage to the growth plate
- Do not use allografts in paediatric ACL reconstruction due to poor clinical outcomes
- Hamstrings which are most commonly used are small and so the options are to:
- Fold over the graft more times in order to make them thicker
- Use hamstring graft from a parent
- Use donor hamstring graft from a cadaver
- Difficulty in restricting activity during the rehabilitation period:
- The younger the child the more difficult it is to:
- restrict their activities
- carry out complex rehabilitation exercises correctly
- rehabilitation exercises therefore need to be tailored to their physical and mental ability to carry them out
How are ACL injuries diagnosed in children?
- The same strategies as an adult should be employed in making the diagnosis:
- History of the injury:
- Typically twisting non-contact injury to knee
- Rapid and large swelling within a few hours
- Examination
- Imaging:
- X-ray – helps exclude fractures
- MRI scan – definitive diagnosis for ACL, cartilage and meniscal injuries
Why is it more difficult to diagnose ACL injuries in children than in adults?
- Children are more difficult historians than adults
- Have greater physiological joint laxity
- X-ray and MRI scans are more difficult to interpret due to developmental variations from adults (e.g. presence of growth plates)
Why do children with ACL injuries have a different injury pattern than adults?
- Children's bones are relatively weaker than those of adults:
- Their bones are less dense and have a lower calcium composition
- As such they are more flexible and likely to bend than break compared to adults
- Ligaments are fibrous connective tissues that attaches bone to bone and as such provide stability across a joint
- Children with ACL injuries have a higher risk of
sustaining an avulsion fracture:
- An avulsion fracture is when a fragment of bone is lifted and separated from the rest of the bone by the ligament or tendon that is attached to it
- Tibial eminence ACL avulsion fracture:
- Children’s ligaments are stronger than the bones and so ligaments can pull off the bone they are attached to
- Children are far more likely to sustain an ACL tibial eminence avulsion fracture (pulling off of the tibial spine where ACL attaches)
- Sleeve fracture of patella:
- This is a particular fracture of the patella only seen in children
- The distal (lower) part of the patella separates from the remaining part
- Caused by rapid forceful contraction of quadriceps against resistance
- Occurs most frequently between 8 and 12 years of age
- It can be difficult to diagnose clearly on X-rays and requires an MRI
- Prompt management is crucial in order to avoid poor long-term effects to knee function:
- Can be managed in a cast if minimal displacement
- Requires surgical fixation if fragments are displaced
- Epiphyseal fracture:
- Growth plates (also called physis) are areas of weakness in a child’s bony skeleton
- Growth plates are composed of cartilage and so are elastic and flexible due to absence of calcium
- They are located at either end of long bones (e.g. femur, tibia)
- Growth plates are part of the bone where new bone formation occurs in children giving bone length and width
- They are therefore responsible for the growth and development of the skeleton
- Fracture lines (where the bone breaks) often go through the growth plate and affect the bone and joint around it
What other injuries are commonly found in the presence of an ACL tear in children?
- Meniscal tear:
- The proportion of the meniscus that has direct blood supply decreases with age
- In adults this is reduced to 10-30% of the meniscus from peripherally going in towards the centre
- As a result, the younger the patient the more likely the meniscus tear will heal following a repair
- Just like in adults there is a one in 6 chance of finding a ramp lesion (separation of the back end of the medial meniscus from the capsule) in those with an ACL injury:
- This requires repair in order to avoid increased stress on ACL reconstruction and risk ongoing knee instability and ACL re-rupture
- Meniscal repair should be performed whenever possible by an appropriately trained surgeon), especially for:
- Bucket handle tear
- Radial tear
- Root tear
- Ramp lesion
- Articular cartilage lesions:
- Should be suspected whenever there is a meniscal tear
- Increased risk of them occurring:
- the longer the time between injury and surgery
- the number of instability episodes from injury to surgery
Rehabilitation following ACL reconstruction in children
- Children are not small adults:
- Exercises need to be modified from the adult rehabilitation protocols so that they can be carried out by the child
- Children need closer supervision when performing exercises so that correct technique can be followed
- Parents need to cooperate and be closely involved with their child’s rehabilitation
- The most important area to focus on is dynamic multijoint neuromuscular control
- Less emphasis is given to strength training in children younger than 12 years
- As the child approaches skeletal maturity the rehabilitation strategies follow more closely those of adults
Focus of rehabilitation
- Exercises that improve dynamic lower limb alignment
- Exercises that improve biomechanical patterns during movement
- Rehabilitation must be thorough and regular
- Progression should be gradual
- Tailor the rehabilitation to the child’s physiology and psychology
- Help mitigate child’s anxiety to re-injury
- Boost confidence in the injured knee
- Promote participation in team training to gain social benefits of being part of a team
- Encourage parental support and involvement throughout the rehabilitation process
Return to sport
- Young athletes and even more so girls have a higher risk of ACL re-injury especially in the first year post surgery
- Need to also train the uninjured leg as there is well documented evidence of increased risk to ACL injury in the other knee
- Injury prevention programme should be incorporated in their training and performed regularly and long term
Complications
- Growth disturbance:
- This is a rare (~2%) but significant risk
- It can lead to:
- Limb shortening:
- This is more obvious the younger the patient is as they have more growth potential left
- Angular deformity:
- This can be in any plane
- The damaged part of the growth plate fails to grow allowing the remaining part of the growth plate to deviate the limb toward the side of where the growth plate damage is located
- Greater potential to occur the more growing the child has left to go through
- Should be followed up with annual X-rays until skeletal maturity and growth plates have closed which is when the child has stopped growing
- Secondary ACL rupture:
- ~25% of patients younger than 25 years sustain a new ACL injury
- ~10% of them occur on the same knee
- ~12% occur in the uninjured knee which is therefore at higher risk of ACL injury
- Risk of knee osteoarthritis:
- Menisectomy is a known risk factor for early osteoarthritis
- This is more pronounced in young patients as they are physically more active
- Meniscal repair is not associated with increased risk of cartilage lesions
- The technical challenges of performing ACL and meniscal repair in young patients means that treatment should be reserved for surgeons who have the experience and perform high volume meniscal repairs
- Knee stiffness:
- This is rare in patients younger than 13 years
- It is associated with the degree of injury to the ACL, capsule and other structures in addition to the ACL, and poor compliance with rehabilitation
- Of paramount importance is the need to have full knee extension prior to ACL reconstruction unless there is a physical block to it such as a displaced bucket handle meniscal tear
- Postoperatively achieving full knee extension is one of the primary aims:
- Failure to achieve this if rehabilitation compliance is not an issue is the possibility of a cyclops lesion:
- This is where a lump of tissue forms at the front of the knee which limits the ability to get the knee fully straight and it necessitates in arthroscopic debridement to achieve full extension
- Infection:
- Whilst this is rare (~0.2%) it’s a serious complication:
- Requires prompt diagnosis and treatment (further information provided in the adult section of ACL reconstruction)